3 Lessons From a Sciatica Misdiagnosis: What Clinicians Should Remember
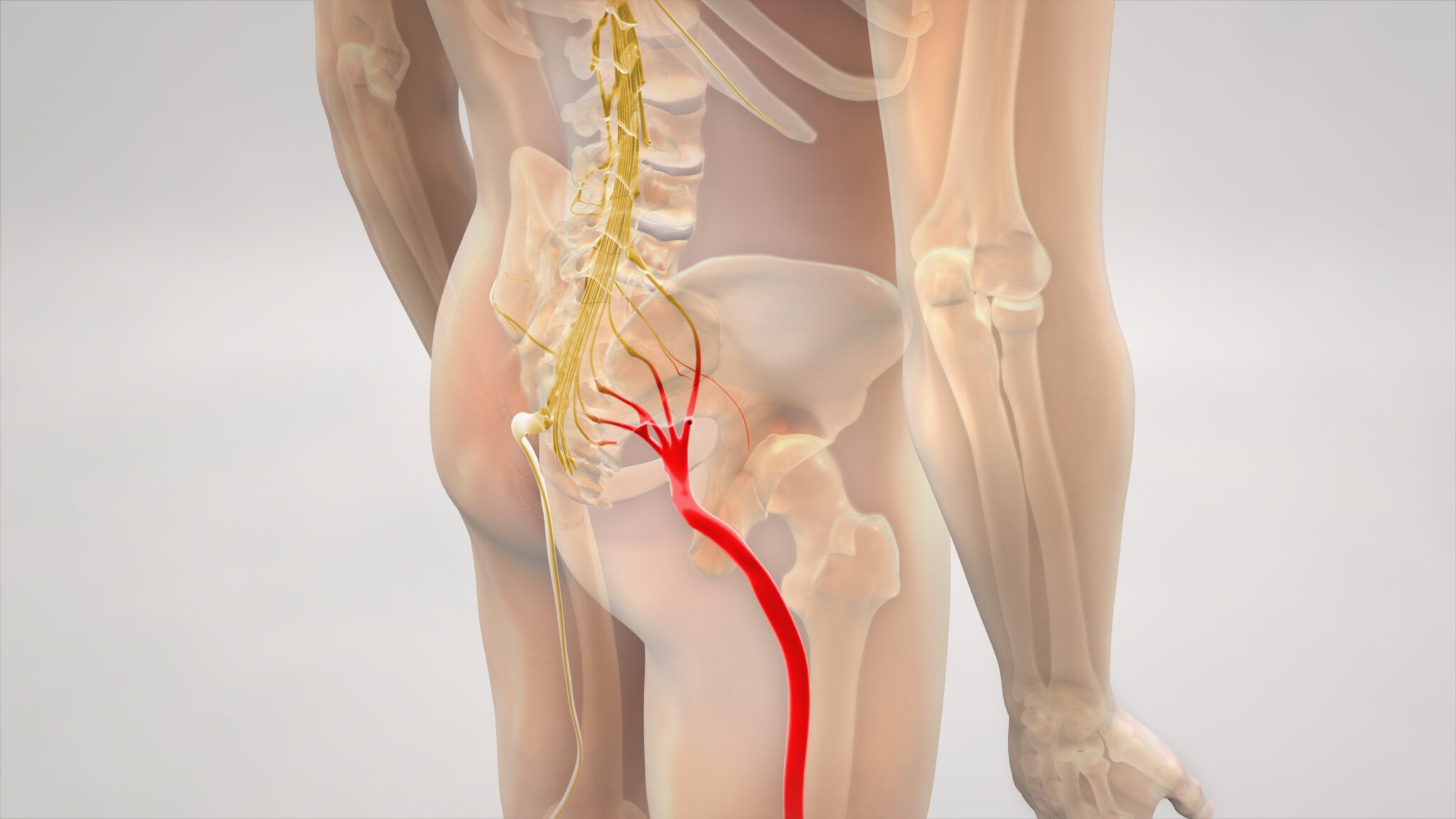
Diagnosing low back and leg pain is rarely straightforward. Even experienced clinicians can be misled when symptoms appear to follow a familiar pattern. A recent case involving a presumed sciatica diagnosis highlights the risk of clinical bias and the importance of maintaining a broad differential.
1. Don’t Get Stuck in “MSK Thinking”
The patient, a man in his mid-50s, presented with low back and leg pain that appeared consistent with sciatica. He had mild neural findings and even a previous history of sciatica, making the MSK explanation feel convincing.
However, the key detail was the predictable exertional nature of his leg symptoms. Pain consistently appeared after walking roughly 150 yards and eased within minutes of rest — a classic feature of Peripheral Artery Disease (PAD).
When symptoms fit the MSK narrative too neatly, clinicians should pause and consider alternative mechanisms.
2. Be Highly Specific in the Subjective Examination
The patient reported pain with bending, lifting, and walking. These are common aggravators in sciatica, but what type of pain occurred during each activity was not clarified.
Important distinctions such as:
- Was it back pain or leg pain triggered by walking?
- How quickly did symptoms settle after stopping?
- Was the pattern predictable day to day?
More specific questioning would have revealed that walking tolerance not spinal loading was the true driver of symptoms.
Additionally, vascular risk screening (“Plaque 5”: smoking, diabetes, dyslipidaemia, hypertension, atherosclerotic disease) was missed. The patient was later found to be a long-term smoker a significant clue.
3. Neural Findings Can Be Red Herrings
Reduced ankle reflex, altered sensation, and a positive straight leg raise can support a sciatica diagnosis, but they are not definitive.
Many patients over 50 with previous episodes of sciatica show mild residual neural findings unrelated to their current complaint. In this case, those findings became misleading anchors.
For PAD, the more relevant objective test is simple: pulse assessment (dorsalis pedis and posterior tibial). A quick vascular screen could have redirected the diagnosis sooner.
Conclusion
This case reinforces that common conditions, not the rare ones often create the biggest diagnostic challenges. Clinicians must maintain curiosity, ask precise questions, and remain open to alternatives even when the initial impression seems strong.
By refining assessment habits and staying alert to key vascular red flags, we can significantly reduce misdiagnosis risk and deliver safer, more effective care to our patients.
References
- Hirsch AT et al. ACC/AHA Guidelines for the Management of Patients With Peripheral Arterial Disease. Circulation. 2006.
- Norgren L et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Journal of Vascular Surgery. 2007.
- Patel MR et al. Low Back Pain and Radiculopathy: Differential Diagnosis. BMJ.
- Jesson T. Case Study on PAD Masquerading as Sciatica. Physio Network, 2024.

